Better lives,through better choices.
Clinical Decision-Making and Case Planning for Children
What is the first clinical decision that needs to be made when working with children?
- The first clinical decision to be made is determining whether the sexual behavior demonstrated by the child is problematic or normative / typical behavior given his or her developmental status.
See Sexual Behavior: Normative or Problematic? and Assessment (Coming Soon) sections to help determine if clinical services are warranted.
What if the sexual behavior appears to be normative or typical?
Parents and other caregivers often ask, “If the sexual behavior is ’normal’ does that mean we should ignore it?” Instead of ignoring the behavior, it is advised that the caregivers see this as a “teachable moment.”
Children can be provided simple rules about relevant topics, including:
- Modesty (“Clothes must stay on, or “Keep private parts covered.”)
- Privacy (“One person in the bathroom at a time.”)
- Interacting with others (“No touching or showing private parts.”)
For more information on Caregiver's Response to Sex Play, click here.
What are some diagnostic considerations for professionals?
Problematic sexual behaviors are not a diagnosable condition. Rather, these behaviors are clinically concerning behaviors. At times, the problematic sexual behaviors represent an isolated problem of a child who is otherwise functioning well. Other times, the sexual behaviors may be part of a pattern of disruptive or delinquent behaviors. Some children with problematic sexual behaviors have also experienced trauma, and the problematic sexual behaviors may be one of the symptoms related to the trauma.
The following section provides guidance for diagnostic consideration, as well as more information about specific diagnoses: American Psychiatric Association Diagnostic and Statistical Manual.
What do I need to know about problematic sexual behaviors as an isolated problem?
Problematic sexual behaviors may be an isolated problem. This is more often the case with older school-age youth (10-12 years old) who may have had exposure to sexualized media and curiosity prompted imitative behavior that was problematic. Puberty can also impact the onset of sexual behaviors.
Disruptive Behavior Disorders
Are problematic sexual behaviors a symptom of disruptive behavior disorders?
- It is not unusual for problematic sexual behavior to be one of the symptoms of disruptive behavior disorders.
- Disruptive behavior disorders are childhood diagnoses that describe characteristics of children that violate societal rules excessively, i.e., beyond what is considered normative. Problematic sexual behaviors involve breaking of rules and violating other people’s physical boundaries and thus may represent behaviors consistent with other symptoms of disruptive behavior disorder(s), such as Attention Deficit Hyperactivity Disorder, Oppositional Defiant Disorder, Conduct Disorder, or Disruptive Behavior Disorder Not Otherwise Specified (NOS). (Coming Soon)
Trauma
Are problematic sexual behaviors related to traumatic experiences?
Problematic sexual behaviors may be directly or indirectly related to traumatic experiences of the child. Many children with problematic sexual behaviors have no history of sexual abuse (coming soon). However, for some children, there appears to be a link between sexual trauma and problematic sexual behavior.
Sexual abuse is more likely to lead to problematic sexual behavior when the abuse included one or more of the following:
- Started when the child was young, such as preschool age,
- Involved penetration,
- Involved multiple perpetrators and/or
- Occurred frequently.
Many children who have experienced a potentially traumatic event do not develop significant symptoms to reach criteria for PTSD, but have difficulties with everyday functioning. Such youth may qualify for a diagnosis of an Adjustment Disorder.
For more information about children’s response to trauma see the website for the National Child Traumatic Stress Network.
What are some other diagnostic considerations that impact treatment and case planning?
- Learning disorders and developmental delays may co-occur in children with problematic sexual behaviors.
- Children with learning disabilities, intellectual disabilities, or developmental disabilities, such as autism, often have difficulties with impulse control. Interpersonal problems can be similar to children with ADHD (as described above), including impulsively touching others’ private parts or violating physical boundaries.
- Playmates of children with developmental disabilities are typically developmentally younger children functioning at a similar level of social emotional development as the older child with developmental disabilities.
- When older children with developmental disabilities begin to have natural curiosities and initiate sex play (particularly when puberty starts), if their playmates are much younger, the resulting behavior is considered problematic and concerning.
How can I develop an individual treatment and case plan?
The diversity of children with problematic sexual behaviors requires individualized treatment and case planning. Treatment and case planning for children with problematic sexual behaviors may include determining:
- If all the children who were involved in the sexual behavior are currently safe and supported.
- What actions are needed to create and maintain safety and support for the children and family?
- Is outpatient community based intervention likely to meet the child and family’s needs, and in the rare cases that it is not, what is the least restrictive placement and treatment environment that will provide timely and effective interventions?
- What treatment modules, elements or interventions best fit the treatment needs of the child and family?
- What developmental, cultural, or other considerations should be integrated in treatment and case planning?
How do I select the most appropriate intervention for the child and family?
Individualized treatment planning accounts for the range of presenting problems (such as ODD, PTSD, learning disabilities) and guides the choice of which evidence-based interventions are most appropriate for the child and family.
Children with problematic sexual behaviors can be broadly grouped into the following categories:
- Children with problematic sexual behaviors only
- Children with disruptive behavior disorder symptoms and problematic sexual behavior.
- Children with PTSD or other trauma reactive symptoms and problematic sexual behavior.
- Children who have complicated histories and clinical presentations with a combination of problematic sexual behavior, PTSD, and disruptive behavior disorder symptoms.
Treatment and planning decisions are based on the severity and the relative level of concern of problematic sexual behaviors compared to other presenting problems.
A single integrated treatment may be preferable to multiple separate treatments, especially where problematic sexual behaviors are secondary priorities.
To what extent should caregivers be involved in treatment?
To be a powerful mediator of change in children with problematic sexual behaviors, parents benefit from learning:
- Effective parenting strategies that promote positive behaviors and reduce misbehaviors (such as praise, time out, behavior charts, supervision, etc.).
- Information about sexual development and guidelines for distinguishing typical sexual behavior from problematic behaviors and origins of these behaviors.
- How to teach basic rules about private parts, sexual behavior, privacy, and modesty, and how to apply these rules to a variety of situations.
- Sex education and address how to promote open communication about sexual knowledge and behavior, as well as address relationship building skills and intimacy.
- Abuse prevention skills, with an emphasis placed on the role and responsibility of caregivers for protecting their children and determining who supervises and interacts with their children.
Engaging caregivers in treatment can be challenging at times. More information is provided here in Intervention, and Parent Engagement.(Coming Soon)
What if problematic sexual behaviors are the main problem?
In cases where problematic sexual behavior is the main or dominant problem, consider research supported short-term cognitive-behavioral treatment protocols designed to treat problematic sexual behaviors. Details regarding the principal components of these interventions are discussed more thoroughly in Intervention, Child , Intervention Types. (Coming Soon)
What are some common elements in research supported problematic sexual behavior focused treatment protocols?
Research supported protocols:
- Are outpatient group treatment program for children and their parents or other caregivers.
- Program can be provided to individual families when group is not an option. (Advantages and Disadvantages of group and family approaches to treatment are described in Intervention, Child, and Modality (Coming Soon).
- Require caregiver involvement and addresses parenting skills, stress, and support.
- Typically take 4 to 6 months, although longer for adolescents.
- Group children by similar developmental ages when group treatment is possible (such as, 3-6 years, 7-9 years, and 10-12 years).
- Are cognitive-behavioral, psychoeducational, and supportive.
- Directly address sexual behavior and are designed to reduce or eliminate incidents of problematic sexual behaviors.
- Include collaborative relationships with child protective services, juvenile justice and court personnel, school personnel, and other involved supports.
What can children and caregivers expect to learn in treatment sessions?
- In sessions, the children learn rules about private parts and sexual behaviors, abuse prevention skills, and receive age appropriate sex education.
- They learn coping and self-control strategies and practice these skills to help them maintain sexual behavior rules and other pro-social behaviors in the future.
- Caregivers are taught how to supervise the children, teach and implement rules in the home, communicate about sex education, and reduce behavior problems utilizing behavior parent training strategies.
How do I select the appropriate level of care?
Outpatient community based intervention is the treatment level of choice for most children with problematic sexual behavior. Higher levels of care are warranted in more severe cases when there is greater potential of harm to the child or others and a need for more intensive intervention than can be provided on an outpatient bases.
Factors to consider include the:
- Willingness and ability of the parents, teachers, and other adults in the child’s life to provide quality close supervision.
- Responsiveness of the youth with problematic sexual behaviors to close adult monitoring, guidance and behavioral redirection and correction.
- Level of aggression, coercion, force and potential harm to self or others.
- Fear, anxiety, and other emotional responses of the other children.
See the Levels of Care & Placement section for more details regarding case planning for placement.
Treatment Approaches for Complex Presentations
How do I treat problematic sexual behaviors with co-occurring disruptive behavior disorders?
- Treatments have strong behavior parent training components and are the treatment of choice for disruptive behavior disorders.
- When the problematic sexual behaviors are the dominant concern, treatment plans starting with a problematic sexual behavior focused approach is an option, with ongoing monitoring of other disruptive behavior disorder symptoms.
- With older children who already have an established pattern of delinquent behaviors and multiple family issues (such as parents with mental health concerns, substance abuse, and barriers to clinic based treatments including poverty, limited transportation and child care options, etc.) then Multisystemic Therapy should be considered if it is available.
- In cases where the pattern of defiant and disruptive behaviors is primary, it may be appropriate to consider using an appropriate, well-supported, evidence-based treatment with problematic sexual behavior-focused components integrated in the protocol.
- Well-supported models such as Parent-Child Interaction Therapy, The Incredible Years, Barkley’s Defiant Child protocol, or the Triple-P program might be considered, integrated with problematic sexual behavior treatment components.
How do I treat problematic sexual behavior and trauma related symptoms?
- Both problematic sexual behavior focused and trauma focused interventions (such as Trauma Focused-Cognitive Behavior Therapy) have been found to reduce sexual behaviors in clinical outcome research. The timing of the trauma related to the onset and progression of problematic sexual behaviors, and the severity of the range of symptoms, help guide these treatment planning decisions.
- If the child is exhibiting other significant trauma related symptoms, particularly re-experiencing symptoms or diagnosis of PTSD, TF-CBT may be the treatment of choice.
- Some children may not have significant internalizing symptoms (e.g., anxiety, nightmares, or depression) or maladaptive attributions associated with the trauma. This absence of specific symptoms may be particularly true in cases where the traumas were distal and not associated with the onset of problematic sexual behavior. In these cases, a problematic sexual behaviors focused approach may be a better fit.
- Trauma focused components could be used as supplements when warranted.
What is the best way to approach treatment of trauma related symptoms, and families with complex social and psychological needs?
- Children with problematic sexual behaviors present with a complicated trauma history with resulting multifaceted concerns at the individual, family, and system levels.
- Focused interventions that blend evidence based protocols with a single therapist are recommended over multiple interventions, providers, and agencies. When components of these interventions are examined, there is significant overlap of treatment components of problematic sexual behavior focused treatment, TF-CBT, and various evidence-based behavior parent training protocols (figure below).
- Assessment driven identification of treatment priorities can facilitate determining treatment components, with ongoing assessment of needs and strengths guiding their order. Often multiple family members have various treatment needs (such as treatment for siblings, caregivers, etc.).
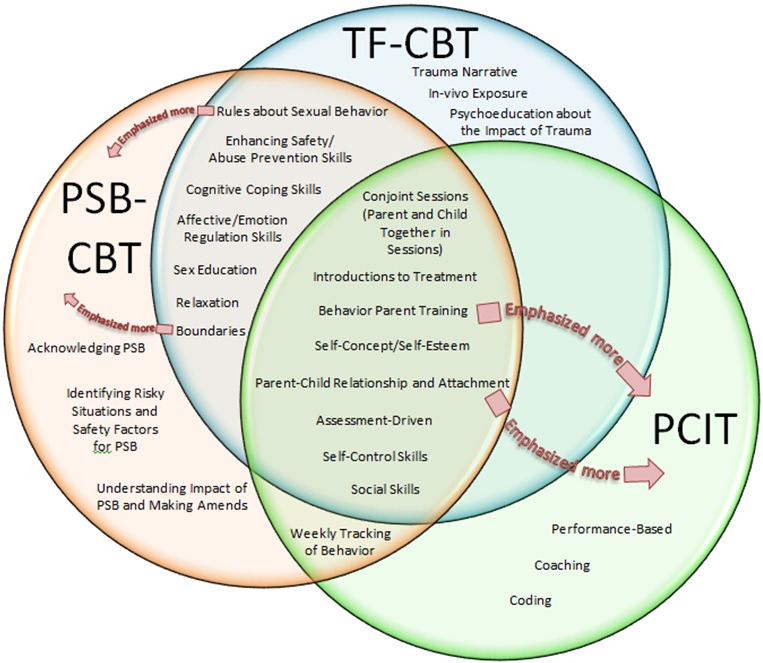
TF-CBT: Trauma Focused Cognitive Behavior Therapy
PSB-CBT: Problematic Sexual Behavior Cognitive Behavior
PCIT: Parent Child Interaction Therapy